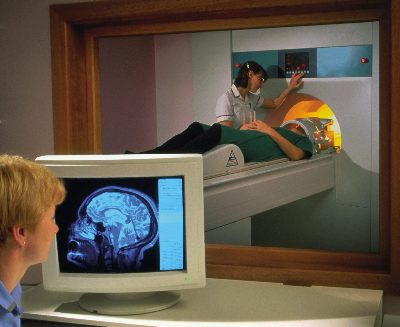
You are likely to be asked to undergo an MRI scan in the course of your MS diagnosis.
MRI images can also be used to monitor relapses and progression.

You are likely to be asked to undergo an MRI scan in the course of your MS diagnosis.
MRI images can also be used to monitor relapses and progression.
An MRI scanner consists of a larger tubular magnet with a bed that slides out from the hole in the middle on which the person being scanned lies.
There are no risks associated with MRI scans, which are painless and generally last from half an hour to an hour, during which time the individual will be asked to lie as still as possible. Some people can find this claustrophobic. Whilst scanning, the machine makes loud banging and buzzing noises. Often people are given headphones to make this more tolerable.
As the scanner is a very powerful magnet, all metallic objects must be left outside the scanning room. It is advisable not to wear clothes with metal poppers, zips or metal buckles.
Unlike CT/CAT (computed axial tomography) scanning , which uses x-rays, MRI creates images by using magnetic fields and radio waves to monitor the behaviour of hydrogen atoms in the body.
The nucleus at the centre of a hydrogen atom spins like a top. The strong magnetic field in an MRI machine (more than 10,000 times stronger than gravity) makes the atoms line up in the direction of the magnetic field.
The machine then fires a pulse of radio waves that causes the atoms to spin in a different direction (causing 'resonance'). When the pulse is turned off, the atoms return to their natural alignment within the magnetic field and release energy. The machine picks up this signal and sends it to a computer, which converts it into an image.
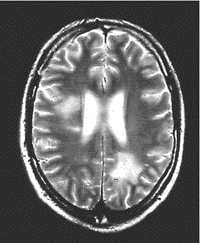
The chemical make up of the scars caused by MS means that they show up as white patches on MRI images, giving a very clear picture of the effects of MS on the brain and spinal cord. By using a contrast enhancing agent called gadolinium, which is injected before the scan, damage to the blood brain barrier can also be identified, which indicates areas of active MS.
Two types of MRI scan are generally carried out when looking for MS lesions, inflammation and loss of neurons.
The main type of scan used in the diagnostic process is known as a T2 image. This is used to determine the total number of lesions or overall disease burden. T2 lesions appear as bright spots on the scan which indicate areas where the myelin sheath has been damaged or destroyed. Changes in the brain due to the ageing process also appear as bright spots on a T2 scan, which is why it can sometimes be difficult to distinguish the lesions seen in MS from the normal changes seen in the brain as a person ages.
Although less useful for diagnosis than a T2 image, the other type of image that can be taken is a T1 image. Areas where nerve cells have been permanently lost or damaged appear as dark areas on this type of scan. A T1 scan can also show areas of swelling (oedema) that aren’t permanent. A contrast dye called gadolinium can be used during a T1 MRI to enhance the sensitivity of the scan. Gadolinium enhancement (GdE) shows areas of active inflammation indicating new lesions or lesions that are becoming larger.
Gadolinium is an inert material used as a marker or contrast agent to enhance images of the effects of multiple sclerosis on MRI scans. When injected before a scan, gadolinium makes it possible to distinguish between active MS lesions and older areas of scarring.
Small amounts of gadolinium may remain in the brain after a scan. In 2017 the European Medicines Agency (EMA) found no evidence that these deposits cause any harm, but recommended using the lowest dose required for a clear image.