What should I do if I think I'm having a relapse?
If you think you're having a relapse, and your symptoms are mild, you might choose to wait and see if they improve. However, if you experience sudden difficulties, such as with your eyesight or mobility, it's more important to contact your MS team as soon as possible in case you need treatment.
Every MS team works differently, so check with your MS nurse or neurologist in advance about what to do if you think you may be having a relapse. Some services have relapse clinics while others will discuss your concerns by phone or email, or book an appointment to see you.
Your MS nurse will ask you about the symptoms you're experiencing, when they started, what has changed and how these symptoms are affecting you on a day to day basis. Your MS nurse will also want to know if there's anything happening that could be making your symptoms worse such as any signs of a possible infection – this will often include having a test for a urinary tract infection (UTI). For women they may ask about your menstrual cycle.
Here are some of the questions the MS nurse may ask.
- When did your symptoms start to change and what has been the pattern of this change?
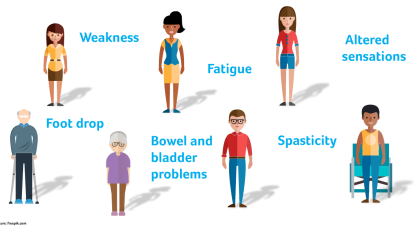
- What symptoms are you experiencing?
- Which part of your body is affected, for example if you have numbness, where is this?
- Have the symptoms stopped you doing anything that you can normally manage, such as preparing meals, driving, getting up and down stairs, working?
- Have you been ill lately or had any symptoms of infection, for example unexplained shivering?
- What medication are you taking and has your medication changed recently?
It'll be easier to answer these questions if you have been keeping track of your symptoms and any drugs you are taking.
Relapses can be a sign that your MS is becoming more active, so it's important to tell your MS team about every relapse even if you don't think you need treatment and that you're generally managing well. This might be an opportunity to raise with them whether you want to continue as you are, or if you want to start explore starting treatment with one of the disease modifying drugs (DMDs). If you're already on a DMD, a relapse could be an indication that it isn't keeping your MS under control, and you might want to discuss whether to continue with this treatment or look at switching to an alternative. Your team need to know about all the relapses you have so they can give you the best information to help you make these decisions.
It can be worrying when you experience a relapse, but try not to panic. It's important to bear in mind that it will usually settle down of its own accord. You know yourself best, so listen to your body.
How are relapses treated?
Once your MS nurse has confirmed that you're having a relapse, they should discuss your symptoms with you and decide whether you need treatment for the relapse itself or any of the symptoms you're experiencing.
Not all relapses need treatment. The symptoms of a relapse will generally improve on their own.
Many MS teams choose not to treat relapses. However, If your relapse is having a significant effect on what you can do day to day, your MS team or GP may suggest you take a short course of steroids. They should discuss with you the pros and cons of taking steroids, so that you can decide together on the best course of action in your particular situation.
Steroids speed up recovery from a relapse by reducing inflammation and, if needed, ideally they should be started as soon as possible after your relapse has been confirmed. However, taking steroids won't affect how well you recover in the long term from the relapse and won’t affect the course of your MS.
You take steroids as tablets, or through an intravenous infusion (drip) in a hospital clinic.
Methylprednisolone is the steroid most often used to treat MS relapses. The NICE MS Guideline recommends the following treatments:
- tablets: methylprednisolone 0.5g daily for 5 days
- iv infusion: methylprednisolone 1g daily for 3–5 days
More information about steroids for treating relapses.
Whether you decide to take steroids or not, there may be other treatments to help you with your symptoms. These might include medication for MS symptoms, physiotherapy, occupational therapy to support you at home or at work, neuropsychology, or speech and language therapy. For more severe relapses, you may need help from social services, for instance with aspects of your personal care or preparing meals.
If required, your MS nurse may arrange a follow-up appointment, which might be face-to-face or over the phone. This will typically take place about two months after the start of your relapse and is an opportunity for your MS nurse to check how you are and for you to discuss other treatment options if things are still difficult. Your MS nurse should also make a record of your relapse and pass this on to your neurologist, so that your MS team has a full record of your relapses and symptoms.
Recovering from a relapse
If you're going through a relapse, it's important to bear in mind that it will usually settle down of its own accord. Recovery is often a case of waiting to see what happens. It's likely that you will feel unwell and more tired than usual while you're recovering from your relapse. This can have an impact both at home and at work. Be kind and don't push yourself too hard during this time.
You might find you're not able to do all the household tasks that you'd normally undertake. Consider asking for some support from family and friends while you're recovering – perhaps help with the cooking, cleaning, shopping, or collecting children from school so you've more time to rest. Asking for help can be one of the hardest things to do, especially if you're used to being independent, but it's likely your family and friends will be happy to help and perhaps just aren't sure what would be most useful – so talk to them!
If you need additional support, talk to your MS nurse. If you are struggling more than usual it may be possible to arrange some social services support, just to help in the short-term. Organisations such as Home Start may also be able to help you cope with family life.
You may need to reduce your hours or take some time off while you're recovering.
Taking time off isn't always easy, or possible, and you might have no alternative but to keep going during a relapse, which can be difficult. If this is the case, it may help to let your manager, human resources/occupational health team, or your education provider know that you're having a relapse. Depending on your needs, it may be possible for them to provide some support or adjustments, such as:
- arranging for you to work from home
- temporarily reducing your hours
- starting work earlier/later to help with fatigue
- providing someone to take notes for you in a lecture or meeting so you can focus on what is being said
- having longer or more flexible breaks during your working day.
Under the Equality Act, you're entitled to ask your employer to make reasonable adjustments to help you remain in work.
If you've had to stop working for a period of time, it's a good idea to stay in regular contact with your manager or human resources rather than just sending in the required paperwork. Keeping people informed will give you the opportunity to talk things through and discuss the best solution for everyone. When you're planning your return to work, it may be helpful to request a phased return, slowly building up the number of hours/days that you work over a period of time.
More information about working with MS.
Relapses are usually unexpected, can take you by surprise and the symptoms can be difficult to deal with, leaving you feeling overwhelmed. This can trigger reactions such as anger that this has happened to you at this particular time, or you may feel that you should've been able to avoid the relapse. You might also have concerns about what the future holds for you or be concerned about the impact that MS will have on your relationships or your work. It's normal to feel emotional, worried or depressed in this situation but try to remember that these feelings won't last forever and they're likely to go away as you recover. If they do become overwhelming, or persist after you recover, you could make an appointment to discuss your concerns with your GP or MS team for some support.
If you're finding it hard to sleep well, you may find it more difficult to deal with everyday situations which wouldn't usually be a problem. Some medications, including steroids, can also have an impact on your emotions.
Relapses can also have an impact on people close to you. Your family and friends may experience a range of emotions such as anxiety, guilt or anger. Being aware that they may have these feelings during a relapse, and that it's a completely normal reaction, can help all of you to manage.
Thinking processes affected
Because a relapse is often stressful, many people can feel distracted and a bit overwhelmed and may have problems thinking through complex tasks. These thinking problems are fairly common during a relapse but should become less of an issue as you recover.
During some relapses, you may have more obvious problems with thinking. You may find that your speed of thinking is slower and that you have trouble concentrating. If these symptoms have come on quite suddenly, it’s possible your relapse is directly affecting your thinking processes – this is called a cognitive relapse.
These symptoms will usually settle down. If they interfere with your ability to do important tasks, an occupational therapist or neuropsychologist can work with you to develop strategies to help you manage. You'll find all sorts of tips and tricks to help with cognitive symptoms on the MS Trust website Staying Smart.
You may have developed new symptoms during your relapse, or been less active which can lead to deconditioning (muscle weakness). Specialist advice and support can help you get back on track with your life.
Can I reduce my risk of having a relapse?
Most people find that relapses happen with little or no warning, though sometimes people can tell when a relapse is 'coming on'. They can happen spontaneously, without any obvious cause and there's nothing you could have done to stop them. However, there are a number of potential triggers which can increase the risk of having a relapse, It's important to look after your general health – this includes your mental wellbeing as well as your physical health – as this could help reduce your risk of having a relapse.
An infection can cause a temporary increase in symptoms (sometimes called a pseudo-relapse) but more serious infections can also trigger a genuine relapse. As flu can trigger relapses, it is recommended that people with MS have an annual flu vaccination.
Lifestyle issues are also important in reducing the risk of relapses. A well-balanced diet and regular exercise will help you stay healthy and reduce the risk of relapse triggers such as infections. Recent studies have shown that smoking increases the relapse rate in people with RRMS, and also increases the risk of disease progression. Smoking could also have an indirect effect as it increases the risk of chest infections, which in turn can trigger relapses.
While some studies have suggested that a prolonged period of stress can cause a relapse, results from other studies have been less clear-cut.
Keeping as healthy as possible will also mean that, if you do have a relapse, you're better placed to recover from it.
Disease modifying drugs (DMDs) should help to reduce the number of relapses you might otherwise have, and also any relapses you do have should be less severe (that is, you are less likely to need steroids or a stay in hospital). Occasionally forgetting to take your DMD will not have much impact but, if you regularly miss taking your DMD, it will not be effective and you may have relapses more frequently. If you have been prescribed a DMD but you're reluctant to take it, perhaps because of its side effects or problems with taking it regularly, you should talk to your MS nurse or neurologist about this.
Relapses may be unpredictable, but you can make sure you're better prepared in the event you do have one. Some of the things you could do include:
- monitoring your MS, noting changes in your symptoms and how they're affecting you. Keeping a log of your everyday MS symptoms can help you and your MS team more easily identify a relapse. Keep a record of any drugs you're taking, the doses and how often you take them. You could keep notes about this in a notebook, diary or an app. Having this information readily to hand can help to make things less stressful when you're not feeling well and need to contact your MS team
- make sure you know who to call if you're worried you may be having a relapse, and what to do if your main contact is unavailable
- build up a support network – you can let people know, that from time to time, you may need help during a relapse. Keep a list of people who can help you such as family, friends, neighbours and work colleagues
- if you have children (especially young children) living with you, you can prepare them for times when you're unwell by encouraging them to take responsibility for chores appropriate for their age and creating opportunities for them to stay away from home overnight or for a few hours at a time. Make a plan together for the unexpected and maybe have a trial run so that your children know exactly what will happen if an unplanned situation occurs
- if you're working, ensure that you are familiar with your employer's policies for sick leave, returning to work, reasonable adjustments and other work-related issues. If you're self-employed but unable to work, make sure you know what benefits you may be entitled to and how to claim them
- stock up on everyday essentials such as longlife milk, food with long use-by dates, a selection of easy meals in the freezer and toilet rolls.
-
Burton JM, et al.
Oral versus intravenous steroids for treatment of relapses in multiple sclerosis.
Cochrane Database of Systematic Reviews 2012;(3):CD006921.
Full article (link is external)
Duddy M, et al.
The UK patient experience of relapse in multiple sclerosis treated with first disease modifying therapies.
Multiple Sclerosis and Related Disorders 2014;3:450-6.
Full article (link is external)
Steelman AJ.
Infection as an environmental trigger of multiple sclerosis disease exacerbation.
Frontiers in Immunology 2015;6:520
Full article (link is external)
Tremlett H, et al.
Relapses in multiple sclerosis are age- and time-dependent.
Journal of Neurology, Neurosurgery and Psychiatry 2008;79:1368-74.
Summary (link is external)
Burns MN, et al.
Do positive or negative stressful events predict the development of new brain lesions in people with multiple sclerosis?
Psychological Medicine 2014;44:349-59.
Full article (link is external)
Artemiadis AK, et al.
Stress as a risk factor for multiple sclerosis onset or relapse: a systematic review.
Neuroepidemiology 2011;36:109-20.
Full article (link is external)
Nickerson M, et al.
Impact of multiple sclerosis relapse: The NARCOMS participant perspective.
Multiple Sclerosis and Related Disorders 2015;4:234-40
Full article (link is external)